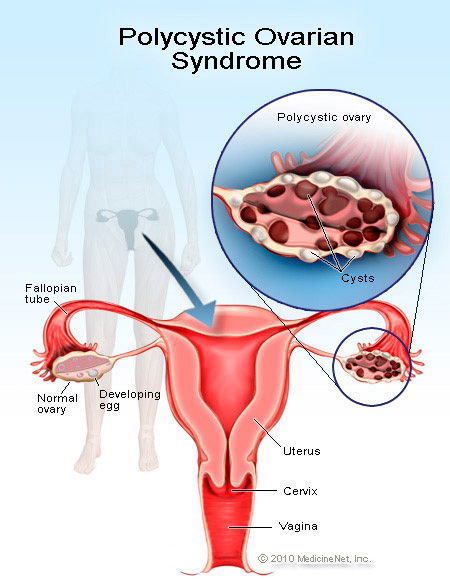
Infrequent or prolonged menstrual periods, excess hair growth, acne and obesity can all occur in women with polycystic ovary syndrome, difficulty becoming pregnant or unexplained weight gain may be the first sign.
The exact cause of polycystic ovary syndrome is unknown. Early diagnosis and treatment may reduce the risk of complications.
Symptoms
Polycystic ovary syndrome signs and symptoms often begin soon after a woman first begins having periods (menarche). In some cases, PCOS develops later on during the reproductive years, for instance, in response to substantial weight gain:
Menstrual abnormality: This is the most common characteristic. Examples of menstrual abnormality include menstrual intervals longer than 35 days; fewer than eight menstrual cycles a year; failure to menstruate for four months or longer; and prolonged periods that may be scant or heavy.
Excess androgen: Elevated levels of male hormones (androgens) may result in physical signs, such as excess facial and body hair (hirsutism), adult acne or severe adolescent acne However, the physical signs of androgen excess vary with ethnicity, so depending on your ethnic background you may or may not show signs of excess androgen. For instance, women of Northern European or Asian descent may not be affected.
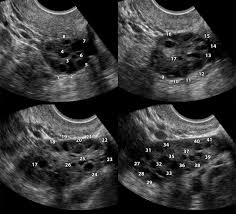
Polycystic ovaries: Enlarged ovaries containing numerous small cysts can be detected by ultrasound. Despite the condition’s name, polycystic ovaries alone do not confirm the diagnosis. To be diagnosed with PCOS, you must also have abnormal menstrual cycles or signs of androgen excess. Some women with polycystic ovaries may not have PCOS, while a few women with the condition have ovaries that appear normal.
Causes
Cause of polycystic ovary syndrome is unknown, but these factors likely play a role:
Excess insulin: Insulin is the hormone produced in the pancreas that allows cells to use sugar (glucose) — your body’s primary energy supply. If you have insulin resistance, your ability to use insulin effectively is impaired, and your pancreas has to secrete more insulin to make glucose available to cells. The excess insulin might boost androgen production by your ovaries.
Heredity: If your mother or sister has PCOS, you might have a greater chance of having it, too. Researchers also are looking into the possibility that mutated genes are linked to PCOS.
Diagnosis
There’s no specific test to definitively diagnose polycystic ovary syndrome. The diagnosis is one of exclusion, which means we consider all of your signs and symptoms and then rules out other possible disorders.
During this process, we take many factors into account:
Medical history.
Physical examination.
Pelvic examination.
Blood tests: Your blood may be drawn to measure the levels of several hormones to exclude possible causes of menstrual abnormalities or androgen excess that mimic PCOS.
Pelvic ultrasound: A pelvic ultrasound can show the appearance of your ovaries and the thickness of the lining of your uterus.
Treatments and drugs
Polycystic ovary syndrome treatment generally focuses on management of your individual main concerns, such as infertility, hirsutism, acne or obesity.
Regulate your menstrual cycle: If you’re not trying to become pregnant, then low-dose birth control pills that contain a combination of synthetic estrogen and progesterone is recommended. They decrease androgen production and give your body a break from the effects of continuous estrogen. An alternative approach is taking progesterone for 10 to 14 days each month. This regulates your periods, but it doesn’t improve androgen levels.
Metformin (Glucophage, Glucophage XR), an oral medication for type 2 diabetes that lowers insulin levels. This drug improves ovulation and leads to regular menstrual cycles.
Pregnancy: If you’re trying to become pregnant, you may need a medication to help you ovulate. Using gonadotropins — follicle-stimulating hormone (FSH) and luteinizing hormone (LH) medications that are administered by injection is the best way to achieve their goal.
Applying IVM procedure for PCOS has great impact on one patient where they used less days less injections and better quality of eggs retrieved give them high success rate.